Tension-Type Headaches
Tension-type headaches are the most common form of headache in adults, with studies suggesting that 30–80% of U.S. adults experience them. These headaches often result from stress, poor posture, fatigue, jaw or neck pain, or dysfunctional breathing patterns.
People often describe the pain as a dull ache or tight, band-like pressure around the head — particularly at the temples, forehead, or the back of the neck. The discomfort can last anywhere from 30 minutes to several days and usually affects both sides of the head, although it may occasionally occur on one side.
Anatomically, this pain occurs because the neck muscles attach to the cervical spine and skull. When these muscles tighten or spasm, they can “tug” on the skull and create tension that radiates into different regions of the head. Depending on which muscles are involved, pain may be felt at the base of the skull, across the forehead, or above the eyes.
Common Muscles That Contribute to Tension Headaches
Upper Trapezius
Sternocleidomastoid
Levator Scapulae
Suboccipitals
Scalenes
These muscles, when tight or overused, can refer pain into the head and mimic classic headache symptoms.
Managing Tension Headaches
Over-the-counter medications such as Tylenol, Advil, Motrin, or Aleve can help relieve symptoms, but it’s important to consult your doctor before use. Always take the lowest effective dose, as overuse can sometimes lead to rebound headaches — a worsening cycle of pain triggered by frequent medication use.
Cervicogenic Headaches
Unlike tension headaches, cervicogenic headaches stem from dysfunction in the upper three cervical spine segments (facet or zygapophyseal joints). Nerves originating in the cervical spine provide sensory and motor information to the head and neck, and irritation of these nerves can produce referred pain that mimics a headache.
Common Identifiers of Cervicogenic Headaches:
Pain primarily on one side of the head (though both sides can be affected)
Restricted neck movement or stiffness
Pain triggered by neck movement or awkward postures
Pain reproduced by pressure at the base of the skull or upper cervical spine
Accompanying same-sided neck, shoulder, or arm pain
Treatment and Outlook
Research shows that neck-specific exercises — particularly low-intensity endurance training — and spinal mobilization can be effective both in the short and long term for managing cervicogenic headaches.
It’s also important to note that not all headaches share the same cause. Some result from dehydration, lack of sleep, or underlying medical issues. Identifying the root cause is the first step toward effective relief — and many cases can be managed without heavy reliance on medication.
In some instances, a local anesthetic injection may be required for pain relief, but this is typically reserved for more severe or persistent cases. Physical therapists can play a crucial role in addressing both tension-type and cervicogenic headaches through posture correction, strengthening, and manual therapy. When in doubt, consult a neurologist or primary care physician to help determine the underlying source of your headache.
Treatment Strategies:
1. Posture Correction & Mobility Exercises
These target stiffness and poor alignment — common triggers for both tension-type and cervicogenic headaches.
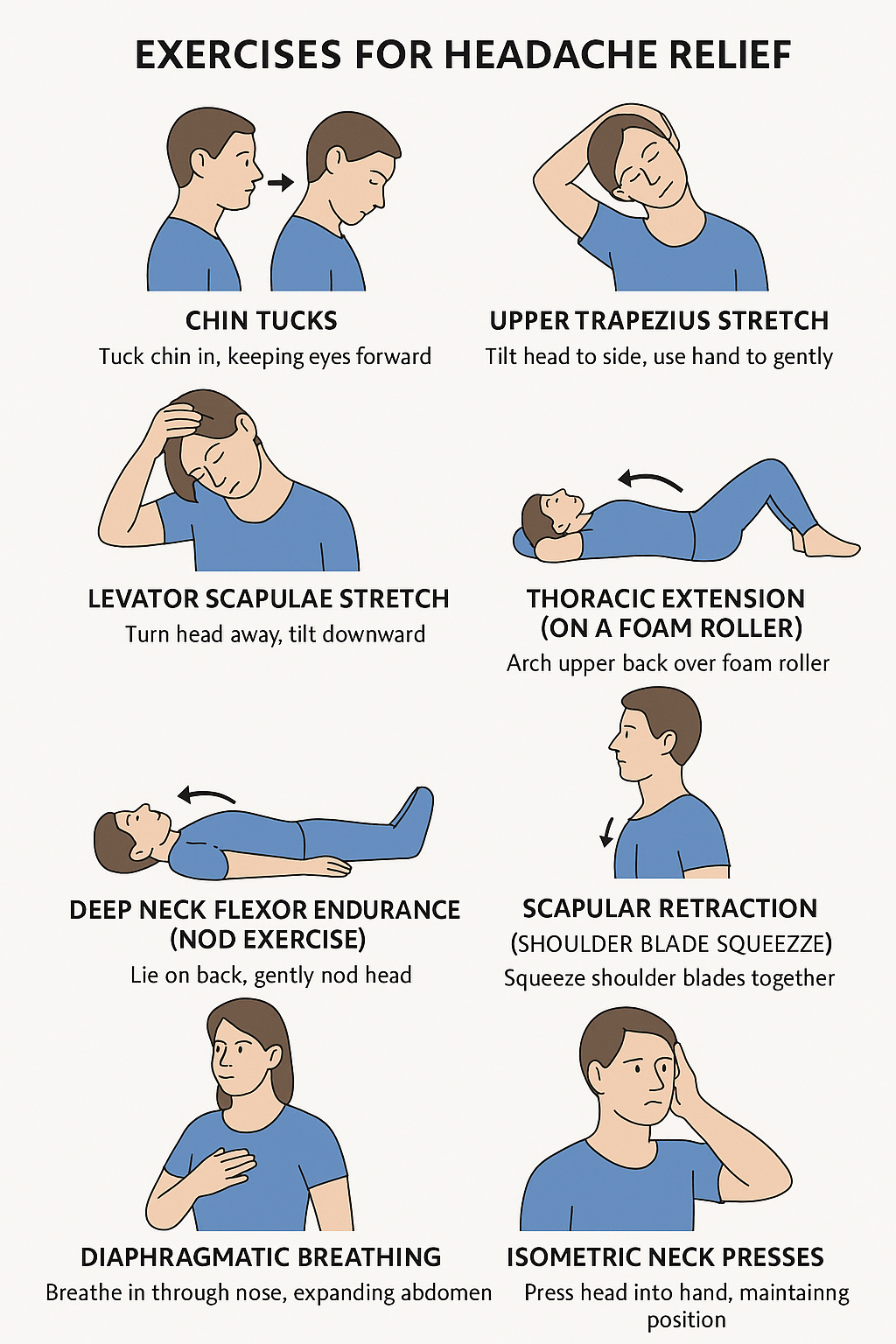
Chin Tucks
How: Sit or stand tall. Gently draw your chin straight back (as if making a double chin), keeping your eyes level.
Hold: 5 seconds
Reps: 10–15
Goal: Strengthen deep neck flexors and counteract forward-head posture.
Upper Trapezius Stretch
How: Sit tall. Gently tilt your head to one side (ear toward shoulder). Use your hand to lightly increase the stretch.
Hold: 20–30 seconds each side
Reps: 2–3 per side
Goal: Reduce tightness in the upper trapezius muscles.
Levator Scapulae Stretch
How: Sit tall. Turn your head 45° to one side, then look down toward your armpit. Use your hand to apply gentle pressure on the back of your head.
Hold: 20–30 seconds each side
Reps: 2–3 per side
Goal: Decrease neck base and shoulder tension.
Thoracic Extension (on a Foam Roller)
How: Lie with a foam roller under your upper back, knees bent. Support your head and gently arch backward over the roller.
Hold: 2–3 seconds
Reps: 10–12
Goal: Improve upper-back mobility and reduce strain on the neck.
2. Neck Strengthening & Endurance Training
These build stability in deep neck muscles that often weaken due to poor posture or prolonged screen time.
Deep Neck Flexor Endurance (Nod Exercise)
Scapular Retraction (Shoulder Blade Squeeze)
Isometric Neck Presses
How: Press your head gently into your hand (forward, backward, side to side) without actual movement.
Hold: 5 seconds each direction
Reps: 5–10 each way
Goal: Build neck stability and reduce muscular fatigue.
3. Breathing & Relaxation Techniques
Dysfunctional breathing and stress can amplify headache frequency and intensity.
Diaphragmatic Breathing
How: Sit or lie comfortably. Place one hand on your belly and one on your chest. Inhale deeply through your nose so your belly rises, then exhale slowly through your mouth.
Duration: 2–5 minutes
Goal: Reduce muscle tension and activate relaxation responses.
4. Daily Habit Fixes
Simple lifestyle adjustments can make these exercises even more effective:
Take movement breaks every 30–45 minutes during desk work.
Keep your monitor at eye level to reduce neck strain.
Stay hydrated and get adequate sleep.
Consider gentle yoga or Pilates to maintain flexibility and posture control.