Low Back Pain and The Contribution of Hip Flexor Weakness
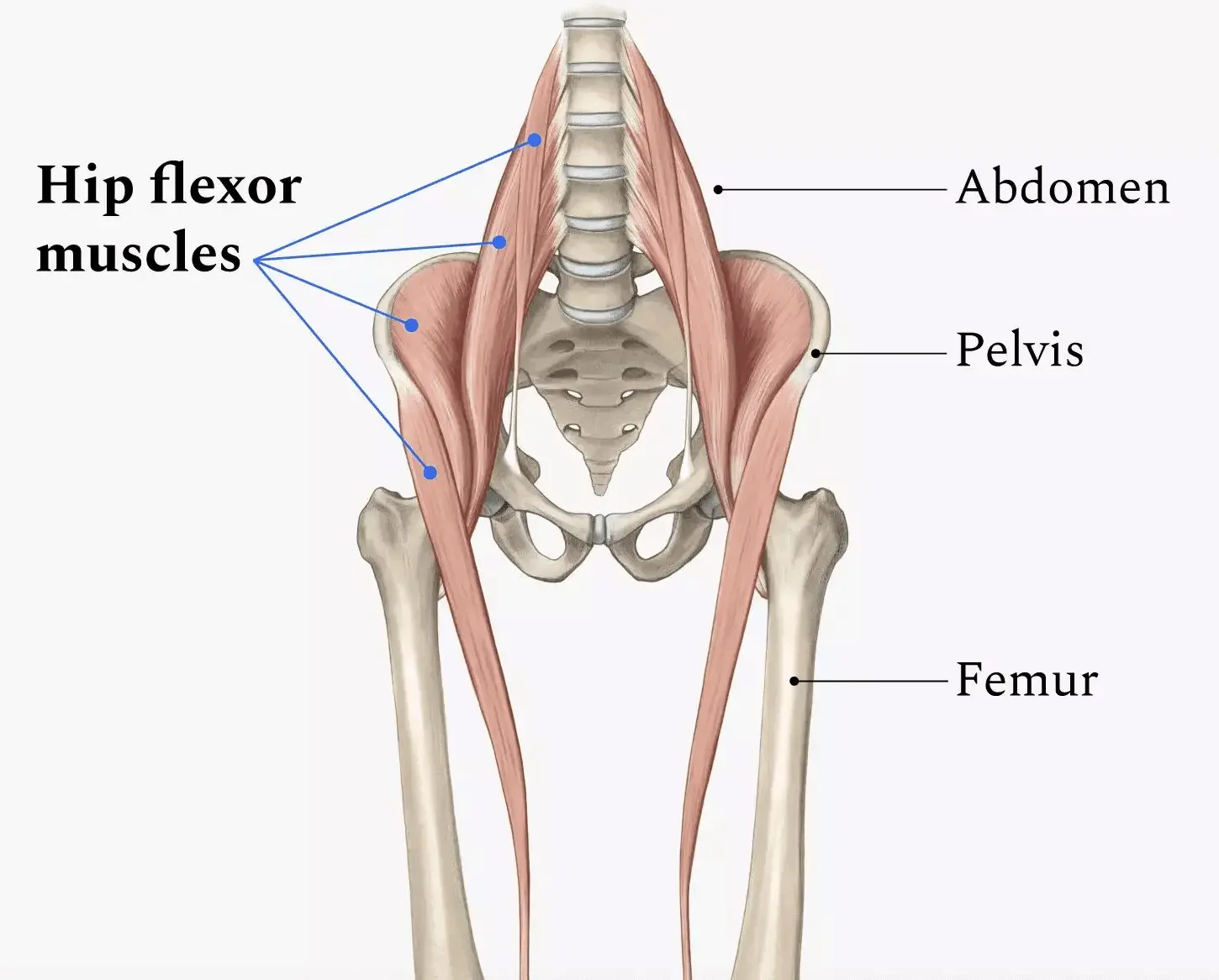
Low back pain is often blamed on the spine itself—but in many active adults, the real driver sits just below it: the hip flexors.The hip flexors (primarily the iliopsoas group) play a major role in controlling pelvic position, stabilizing the spine during movement, and efficiently transferring force between the upper and lower body. When these muscles are weak—not just “tight”—the low back is often forced to compensate.The Hip Flexors’ Role in Spine Support
Hip flexors don’t just lift your leg. They help:Maintain proper pelvic alignmentAssist with trunk stability during walking, running, and liftingControl excessive lumbar extensionWhen they’re strong and functioning well, they reduce unnecessary stress on the lumbar spine
What Happens When Hip Flexors Are Weak
Hip flexor weakness can lead to:Increased lumbar overuse: The low back muscles work harder to stabilize and move the bodyAltered movement patterns: The spine substitutes for hip motion during activities like running, squatting, or getting up from a chairPoor load distribution: Forces that should be absorbed by the hips shift to the lumbar spine
Over time, this compensation can contribute to stiffness, muscle guarding, flare-ups, or persistent low back pain.Why Stretching Alone Often Falls Short
Many people focus on stretching hip flexors when back pain shows up. While mobility matters, stretching without addressing strength can actually worsen instability. A muscle can feel “tight” because it’s weak and overworked—not because it needs more length.The Fix: Strength With Intent
Improving hip flexor strength—especially through controlled, functional movements—helps:Restore proper pelvic controlReduce excess lumbar motionImprove efficiency during sport and daily activity
When the hips do their job, the low back doesn’t have to.Bottom Line
Low back pain isn’t always a back problem. Weak hip flexors can quietly drive compensation, overload, and recurring symptoms. Addressing strength—not just flexibility—can be a key step toward lasting relief and better movement.If back pain keeps coming back despite stretching and rest, it may be time to look at how your hips are contributing.Looking for Lasting Relief From Low Back Pain?
Low back pain is one of the most common reasons people seek physical therapy, especially among active adults, athletes, and individuals with recurring flare-ups. If you’ve tried rest, stretching, or general exercises without lasting results, the issue may not be your spine alone. At JSR we evaluate the entire movement system—especially the hips—to identify strength deficits and movement patterns that contribute to ongoing low back pain. A targeted, individualized approach can help reduce pain, restore function, and keep symptoms from coming back.Below are Exercises that Target the Hip Flexors. They are ordered from easiest to the most difficult. Start with the easiest exercises and work towards the harder ones but take your time with it. It could take months before you work towards the pikes.Start with 2-3 sets of anywhere from 6-20Make sure to always prioritize form over repsDry Needling: How It Helps Reduce Pain and Speeds Up Healing
If you struggle with muscle tightness, nagging pain, or stubborn trigger points that never seem to relax, you may have heard your physical therapist mention dry needling.Dry needling is a proven, research-supported technique used in many sports and orthopedic physical therapy clinics to help decrease pain, improve mobility, and speed up recovery — especially when traditional stretching and massage alone aren’t enough.At JSR, we use dry needling as part of a comprehensive, one-on-one treatment approach to help active adults and athletes move better and feel better — safely.What Is Dry Needling?
Dry needling involves inserting a very thin, sterile filament needle into tight or irritated muscles (often called trigger points).These trigger points can:Cause aching, burning, or sharp painLimit mobilityCreate “tightness” that always comes backRefer pain into other body regions (for example: neck pain creating headaches)
Unlike acupuncture — which is based on Eastern medicine energy pathways — dry needling is rooted in modern musculoskeletal science and focuses on:Resetting irritated nervesReleasing muscle tensionImproving blood flowCalming pain signals in the nervous system
How Does Dry Needling Help Reduce Pain?
When the needle reaches the trigger point, the muscle often produces a small, quick twitch. That twitch response helps “deactivate” the trigger point.Afterward, many people experience:✔ less tightness
✔ improved movement
✔ reduced pain
✔ easier muscle activation during exerciseDry needling can help with conditions such as:Low back painNeck stiffness and headachesShoulder painTennis/golfer’s elbowHip painKnee painChronic tight calves or hamstringsSports injuriesPost-surgical tightness
The key: dry needling isn’t done alone. It works BEST when combined with manual therapy and specific strengthening — so the pain relief actually lasts.Is Dry Needling Safe?
When performed by a licensed and trained physical therapist, dry needling is considered very safe.Most people feel:Potentially mild soreness for 12–24 hoursa sense of muscle “release”Easier movement shortly afterward
Dry Needling and Physical Therapy: Why They Work Well Together
Dry needling can quickly calm painful muscles — but the long-term change comes from retraining the way your body moves.That’s why, at JSR, dry needling is paired with:Corrective strength trainingMobility and stability workEducation on movement and load managementSport-specific rehab
The goal isn’t to “chase pain.”
The goal is to address the root cause so you can get back to the activities you love.Who Can Benefit?
Dry needling may be helpful if you are:An athlete dealing with recurring tightnessAn active adult dealing with work-related painReturning from injury and struggling with muscle tensionDealing with chronic pain that hasn’t improved with stretching alone
If you’re unsure whether it’s right for you, a physical therapist can evaluate your movement, strength, and symptoms first.If you’re looking for dry needling or sports-focused physical therapy in Winter Springs, Winter Park, Orlando, or surrounding Central Florida areas, we’d love to help.Our one-on-one approach ensures every session is tailored to you — not a template.Schedule an evaluation to find out whether dry needling may help reduce your pain, improve mobility, and get you back to moving comfortably again.Pickleball Injury Risks & Player Demographics: What Athletes Should Know
Pickleball has exploded in popularity in recent years, drawing players from all age groups and fitness levels. While it’s a fun way to stay active and social, the sport does carry a notable risk of injury — especially for certain age groups and competitive levels. Understanding the statistics and common injury trends can help players stay safer and enjoy the game for years to come.Why Injury Risk Is Rising
Pickleball-related injuries in the United States have increased substantially over the last decade as more people take up the sport. From 2013 to 2022, the number of pickleball injuries presenting to U.S. emergency departments jumped dramatically, with tens of thousands of players seeking care each year. In 2022 alone, about 13,690 pickleball-related injuries were estimated in U.S. emergency departments — a dramatic rise compared with earlier years.
PMC
Research also shows injury numbers increased sharply during the pandemic years, likely due to more people playing recreational sports and expanding participation across age groups.Who Is Getting Hurt?
One of the most consistent findings in pickleball injury data is the age distribution of players who get injured: A large majority of pickleball injuries occur in players aged 50 and older, with some studies finding that 87–90% of emergency room visits for pickleball injuries involve adults over 50.National injury surveillance data also show that most injury cases occur in players between 60 and 79 years old, reflecting both the popularity of pickleball among older adults and age-related physical risks.It’s worth noting that while older players tend to represent the highest numbers of injuries, middle-aged and younger adult players still face significant risk, especially if playing frequently or without proper preparation. One study found injury prevalence ranged from nearly 50% in younger adults (18-32 years) to over 77% in 48-62-year-olds.
What Types of Injuries Are Most Common?
1. Acute injuries
– Fractures and falls are surprisingly common, especially among older players. Several injury datasets report fractures making up around 27-30% of pickleball injuries, particularly wrist and upper extremity fractures.2. Soft-tissue injuries
– Sprains, strains, and muscle injuries are also frequent, particularly involving the legs and ankles — likely due to quick lateral movements and sudden stops typical of pickleball play.Other injury types include shoulder and elbow issues (“pickleball elbow”), Achilles and knee injuries, and even eye injuries — with over 1,200 pickleball-related eye injuries reported in one recent study.Why These Injuries Happen:
Injury risks in pickleball aren’t random — they stem from a combination of factors:Sudden and multi-directional movements: Quick lateral shuffles and abrupt stops can stress joints and soft tissue.Falls: Loss of balance or unexpected slips are very common, especially on uneven surfaces or in older adults.Repetitive motion: Repeated swings and cutting movements can overload muscles and tendons over time.Lack of preparation: Many players skip adequate warm-ups, strength work, or mobility training — increasing risk.
These factors underscore why proper physical preparation and recovery are essential for pickleball longevity.Average Player Age Matters
Although specific national surveys vary, pickleball’s player base has been trending younger as the sport spreads. According to industry reports, millions of Americans now play pickleball — and the average player age has been reported in the mid-30s, reflecting its growing appeal beyond traditional “senior sport” demographics.However, even when the average age includes many younger players, injury risk remains disproportionately high among older adults, largely due to age-related changes in balance, bone density, and muscle strength.What This Means for You
Pickleball can be an excellent way to stay fit and active at any age. At the same time, awareness of injury risk is critical. Knowing the trends — such as higher injury rates in older players and common fracture and sprain patterns — helps players and clinicians alike make smarter training choices.
Physical therapists can play a key role in injury prevention and recovery, focusing on:Strength and balance trainingMovement mechanics and injury reduction strategiesWarm-up, cool-down, and recovery protocols
If you experience pain during or after pickleball play, or if you want a personalized training plan to reduce your injury risk, consider consulting a sports-focused physical therapist — especially before symptoms become more serious.When “Tight Muscles” Are Actually Weak
Why Stretching Isn’t Always the Answer
Feeling tight is one of the most common complaints we hear in physical therapy. Tight calves, hips, hamstrings, shoulders, or low backs often lead people to stretch more and more, hoping for lasting relief.I personally hear this all of the time regarding the hamstrings. And, in most cases, I find that a lot of these patients have good hamstring flexibility which my patients are shocked to hear.So what does it mean when a feeling of muscle tightness isn't a flexibility problem?In many cases, a muscle feels tight because it is weak, fatigued, or unable to handle the demands placed on it. And when weakness is the real issue, stretching alone rarely solves the problem long-term.Why Muscles Feel Tight in the First Place
Muscle tightness is not always about lack of length. It can be a protective response from the nervous system.When a muscle lacks strength, endurance, or control, the body may increase tension in that area to create a sense of stability. This makes the muscle feel stiff or restricted, even though it may not actually be shortened.This is especially common in active individuals who train frequently, sit for long hours, or return to activity after injury.3 Signs Your “Tightness” May Actually Be Weakness
1. Tightness Gets Worse With Activity
True muscular stiffness often improves once you warm up. If a muscle feels progressively tighter, more fatigued, or more uncomfortable during workouts or sports, it may be struggling to keep up with the load being placed on it.Weak muscles often tighten as a protective mechanism when they are being overworked.2. The Same Muscle Feels Tight After Every Workout
If you constantly feel tight in the same area after every training session, run, or game, flexibility is unlikely to be the main issue.Recurring tightness in the same spot often means the muscle lacks the strength or endurance required for your activity, causing it to fatigue quickly and tighten repeatedly.3. Stretching Only Provides Short-Term Relief
If stretching helps for a few minutes or hours but your tightness quickly returns, this is a strong clue that stretching alone is not addressing the root cause.Stretching can temporarily reduce tension, but it does not increase load tolerance or control. When a muscle is weak, the sensation of tightness often returns as soon as you begin moving again.Why Stretching Alone Doesn’t Fix Weakness
Stretching is a useful tool and can be useful temporarily (while you are addressing muscle weakness,) but it doesn’t improve strength, stability, or movement control.If a muscle cannot handle the demands of your sport, workouts, or daily activities, it will continue to tighten no matter how much time you spend stretching. Over time, this can lead to:Ongoing discomfort or stiffnessRecurrent injuriesReduced performanceCompensations in nearby joints or muscles
Without addressing strength and movement, tightness often becomes a recurring cycle.When Strengthening Is the Missing Piece
Targeted strengthening helps muscles:Tolerate load more efficientlyImprove coordination and enduranceReduce unnecessary tensionSupport joints more effectively
When strength and control improve, muscles often stop “guarding,” and the sensation of tightness naturally decreases — sometimes without additional stretching at all.This is why many people feel looser and better after consistent strengthening, even if they stretch less.When adding strengthening to address weakness, make sure to hit each problem muscle 2-3x/week for 2-3 sets of anywhere between 8-15 reps.Why Proper Assessment Matters
Not all tightness needs stretching. Sometimes it needs strengthening.Determining which approach is appropriate requires evaluating strength, movement patterns, joint mobility, and how your body responds to activity. Treating every tight muscle the same way can lead to frustration and stalled progress.A physical therapist can identify whether tightness is coming from true mobility restrictions, muscle weakness, or movement inefficiencies — and create a plan that actually addresses the cause.The Hidden Cost of “Playing Through” an Ankle Sprain
Why Rest & Recovery Matter
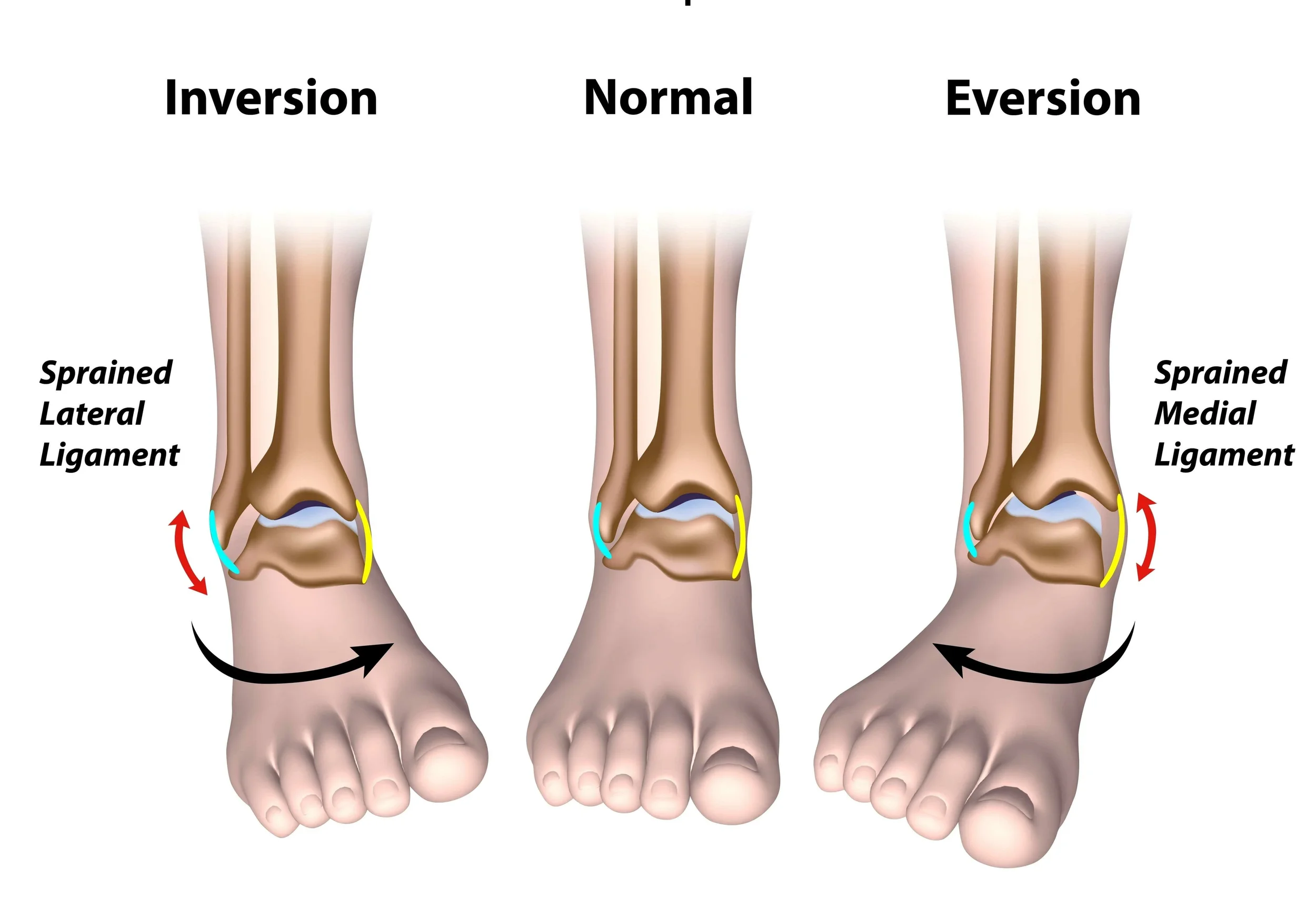
An ankle sprain is one of the most common injuries in sports — and one of the most ignored.An ankle sprain occurs when the ligaments that support the ankle joint stretch or tear — often from a twist, awkward landing, or sudden change in direction. While it might be tempting to “tough it out,” especially for athletes or dedicated weekend warriors, skipping proper recovery can have long-term consequences.Many athletes treat it like a minor inconvenience: tape it, lace up tight, and keep playing. While that mentality might feel tough in the moment, playing through an ankle sprain without proper rest and recovery can lead to long-term problems that are far harder to fix than the original injury.Most Common Sports for Ankle Sprains (and Why Athletes Are at Risk)
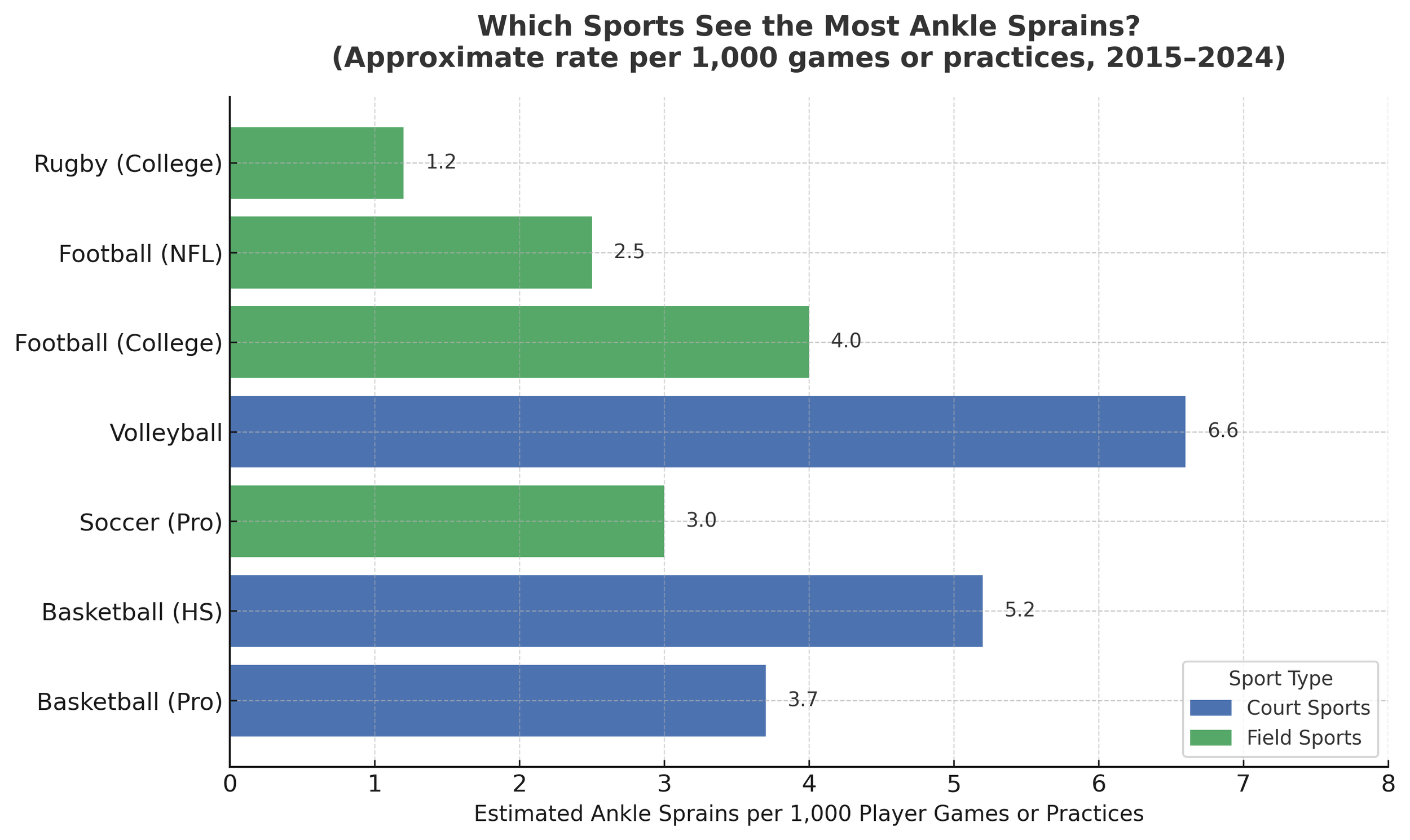
Ankle sprains are especially common in sports that involve jumping, rapid changes of direction, cutting, or contact — movements that stress the ankle joint repeatedly or unpredictably.Here are some of the top sports and statistics:
Basketball consistently shows among the highest ankle-sprain rates. In one study, the ankle-injury rate was ~3.85 per 1,000 participations.Soccer is frequently listed among the top sports for ankle sprains, due to cutting, pivoting, and contact.Volleyball players face higher ankle sprain risk (especially high ankle-sprain risk vs the traditional inversion ankle sprain) because of jumping and landing, especially at the net.Indoor/court and team sports broadly (handball, field hockey, netball, etc.) — A broad review found that ankle sprains are among the most common injuries across many sports — particularly those involving court play, quick direction changes, or jumping.
At the collegiate level, foot and ankle injuries (with ankle sprains the most common) often account for a substantial portion of all injuries — especially in disciplines involving jumping and changes in directionBecause athletes in these sports frequently push through minor injuries or “shake off the pain” to keep playing, ankle sprains often go under-treated — which can lead to a cascade of future problems.Long-Term Implications of Skipping Proper Recovery
Neglecting recovery or returning to sport too early after an ankle sprain can lead to several negative long-term outcomes:Chronic Ankle Instability (CAI): Up to ~20% of people who suffer an acute ankle sprain go on to develop CAI; other studies suggest recurrent sprains and persistent symptoms in 40–70% of cases.With CAI, the ankle can repeatedly “give way,” leading to further sprains, swelling, and functional limitations.Post-traumatic osteoarthritis (PTOA): Repeated or poorly healed sprains can cause joint cartilage damage, early wear and tear, and eventual arthritis — even in relatively young athletes.Altered biomechanics, secondary injuries: To compensate for a weak or unstable ankle, people often change their gait or movement patterns — which can overstrain other joints (knees, hips, back) or lead to chronic stiffness in the ankle.Reduced performance & quality of life: Chronic pain, instability, or limited mobility can interfere with athletic performance, daily activities, and long-term physical health.
How Proper Recovery + Rehab Helps:
Allows ligaments to heal properly — Controlled rest, protection (bracing or limited weight-bearing if needed), and gradual rehab give the injured ligaments time to scar in and regain strength.Restores stability and proprioception — Rehab should include exercises for range of motion, strength, balance, and neuromuscular control. This is crucial for preventing re-sprains or instability.Prevents chronic issues — By allowing proper healing and retraining the supporting muscles/joints, you significantly reduce risk of chronic instability, arthritis, and long-term impairment.Prepares you safely for return to sport or activity — Rather than jumping back in too soon and risking re-injury, a full recovery gives you the best chance of returning at full strength with reduced long-term risk.
An ankle sprain may seem like a short-term setback, but how it is managed early can greatly influence long-term movement, performance, and joint health. Allowing the ankle to fully recover helps restore strength, stability, and confidence while reducing the risk of future injuries. Working with a physical therapist ensures that recovery focuses not only on pain relief, but on rebuilding proper movement and preparing the body for a safe return to sport or daily activity.Why Grip Strength Matters in Baseball Players
Grip Strength: The Secret Link to Velocity, Control & Shoulder Health
Grip strength might be the simplest but most overlooked metric in overhead athletes — especially baseball players.It predicts shoulder stability, elbow stress, velocity, and even how efficiently energy transfers through the throwing chain.Overhead athletes generate enormous force through the kinetic chain — from the ground → hips → torso → shoulder → elbow → wrist → hand.The hand is the final link in that chain.If grip strength is low or imbalanced, the entire chain becomes less efficient… and less safe.So How Exactly Does Grip Strength Help?
1. Grip Strength = Shoulder Stability
During throwing, the rotator cuff fires intensely to stabilize the humeral head.
But research in biomechanics shows that distal stability (forearm & grip) reduces proximal load.
Stronger grip =More co-contraction of rotator cuffBetter humeral head controlImproved dynamic stabilityLess stress on the labrum and capsule
A stronger grip helps protect the shoulder during high-velocity throwing.2. Grip Strength Correlates With Velocity & Control
A stronger grip improves:Wrist stiffnessEnergy transfer at ball releaseSpin rate & command
Pitchers with higher grip strength often demonstrate:Higher velocityMore stable release pointReduced elbow varus torque
3. Grip Strength Protects the Elbow (UCL)
UCL stress peaks during late cocking and acceleration. A strong grip improves forearm flexor-pronator activation — the natural dynamic protectors of the UCL.Low grip strength = increased UCL load = higher injury risk.How Can We Test Grip Strength:
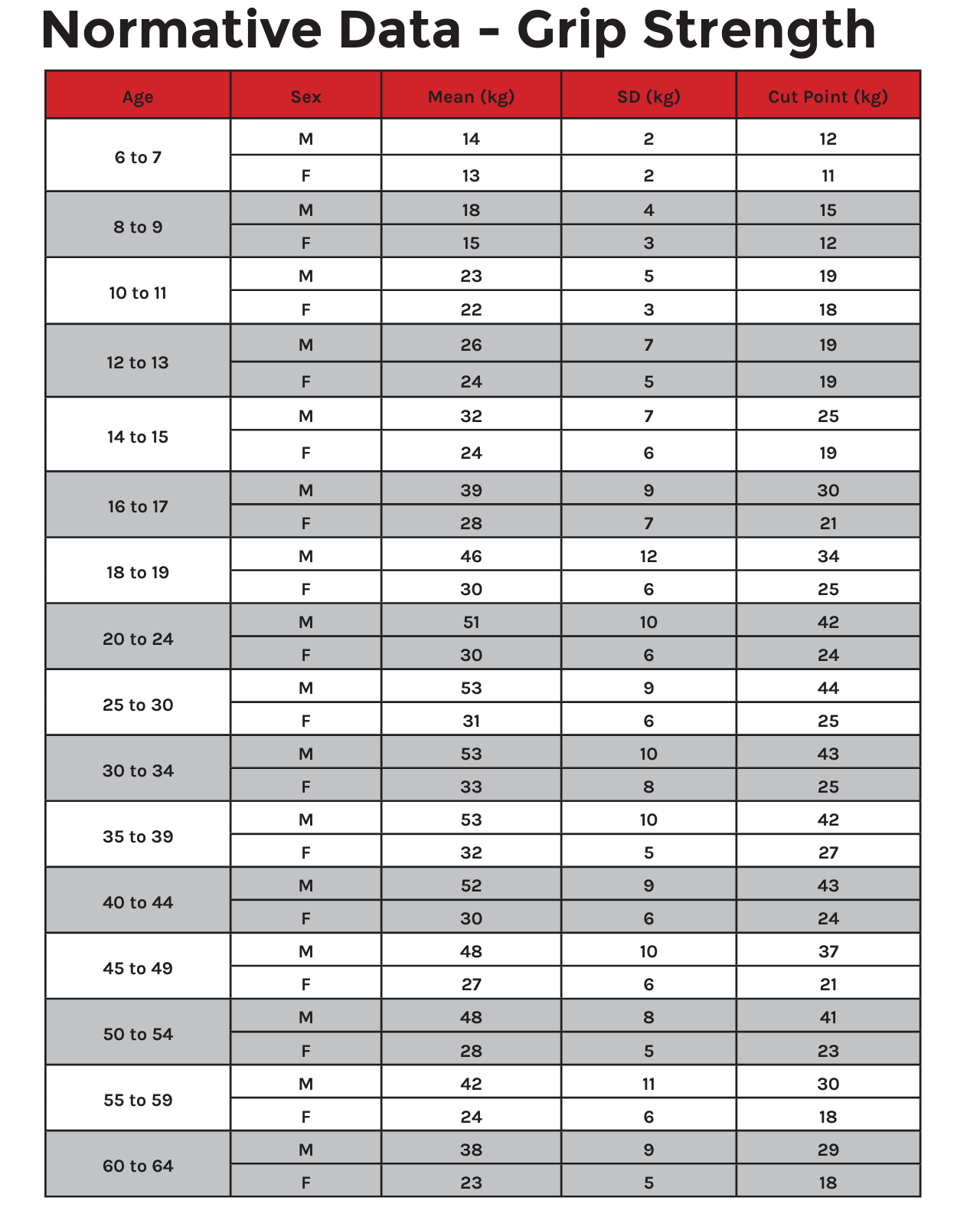
We typically test grip strength using a device called a dynamometer. These devices can be inexpensive with some $30 options on amazon. It is ideal to test grip strength in 2 positions:Arm at the side of the body with the elbow bent to 90degreesArm straight overhead
To determine left to right grip strength you take 3 maximal effort squeezes of the dynamometer in each position on each hand. Add the 3 numbers together then divide by 3 to get the average in each position. You can then compare these measurements left to right and overhead to down at the side of the body.Why Test Grip Strength Overhead?
Testing overhead simulates the functional throwing position where the shoulder is externally rotated and elevated — the exact moment when:Rotator cuff demand is highestGrip-forearm-shoulder linkage matters mostInjuries frequently occur
The Key Rule: Grip Strength Overhead Should Be ~2% Stronger Than at the SideBecause in overhead position the rotator cuff and scap stabilizers engage more. This increases neuromuscular drive through the kinetic chain → producing a small but measurable strength boost.The 2% Rule
If overhead grip strength is roughly 2% stronger than grip at the side → NORMALIf overhead grip = SAME or WEAKER → Red flagPossible cuff inhibitionScapular dyskinesisPrevious shoulder or elbow irritationPoor energy transferIncreased injury risk
Normative Grip Strength Values: Provided through FMS
The Grip testing mentioned above is just one of many tests we perform on our baseball players to ensure that the whole body is functioning cohesively as a unit. There are many other body parts to look at to ensure too much stress isn't going to the elbow or shoulder such as hip mobility, core strength, pelvic control, single leg balance and strength, etc.
And I know we focused on Baseball, but grip strength is important in all overhead sports whether its volleyball, tennis, pickleball, football, etc.
If you would like to be screened due to pain or a history of pain, let us know!Shoulder Injuries in Swimmers — What Every Swimmer & Coach Should Know
Swimming is a fantastic sport for cardiovascular fitness, endurance and whole-body conditioning. But despite being low-impact on joints compared to many land sports, swimmers face very high rates of shoulder problems. Because every stroke uses the shoulder repeatedly — often thousands of times per week — subtle overload, technique flaws or muscle imbalances can add up.At JSR, we see many swimmers with shoulder pain, and it’s our goal to help you recognise, prevent and manage these injuries so you can stay in the pool strong and pain-free.How common is shoulder pain/injury in swimmers?
A recent systematic review found reported rates of shoulder injuries among competitive swimmers between 40% and 91%, depending on study design, age and competitive level. MDPI+2journal.aspetar.com+2In a survey of youth swimmers aged 9-17 in the U.S., 49% reported shoulder symptoms that impacted their swimming. PMC+1One 2014 article stated that shoulder injuries are the most common injuries in swimming, with prevalence in many studies from 47% to 90%. journal.aspetar.comAmong highly trained swimmers, one study reported 74% had experienced at least one shoulder injury, and more than half of those had a recurrence. British Journal of Sports Medicine
The takeaway: shoulder issues are very common in swimmers, not just the occasional problem. Recognising the risk and taking proactive steps is key.Why do swimmers get shoulder injuries so often?
Here are some of the major contributing factors:Repetitive overhead motion – Freestyle, butterfly and backstroke all involve repeated overhead or near-overhead arm movements, putting the shoulder in vulnerable positions for long periods. journal.aspetar.com+1High training volume – Elite swimmers sometimes complete thousands of arm rotations per day. That repeated load accumulates. PMC+1Technique flaws – Small inefficiencies in stroke mechanics (for example poor body roll, incorrect entry, hand path) can increase shoulder stress. journal.aspetar.comMuscle imbalances / fatigue – If the shoulder stabilisers (scapular muscles, rotator cuff) are weak or fatigued, then the larger muscles take over and strain increases.Training load spikes – Rapid increases in volume or intensity (new sets, more distance, hand paddles or drag devices) are often tied to onset of pain. journal.aspetar.com+1Prior injury – A history of shoulder pain is one of the strongest risk factors for new or recurring shoulder injury. PMC+1
The most common shoulder injuries in swimmers:
1. Swimmer’s Shoulder (Overuse Impingement)
Often called “swimmer’s shoulder,” this is really a pattern of overload, irritation or impingement of the rotator cuff tendons (especially the supraspinatus) and related structures. The term is broad but useful.
journal.aspetar.com
+1
What to look for: Pain with the catch or pull phase of stroke, soreness after training, sometimes pain in daily life if it’s progressed.
2. Rotator Cuff Tendinopathy / Tendinitis
With constant repeated motion, the rotator cuff (the small stabilising muscles of the shoulder) can develop tendon irritation or degeneration. Over time it can become a chronic issue rather than an acute tear.
Key issues: Weakness in external rotation, pain with resisted movements, fatigue of the shoulder late in training.
3. Labral Injuries (e.g., SLAP tear)
The labrum is the ring of cartilage around the shoulder socket; in some swimmers, repeated overhead stress or subtle instability can cause fraying or tearing of the labrum.
Signs: Deep-shoulder pain, catching or clicking, decreased power in strokes, sometimes a feeling of looseness.
4. Shoulder Instability / Multidirectional Instability
Some swimmers develop too much laxity or movement in the shoulder joint (often because of high training loads + technique demands) which leads to pain, micro-trauma and inefficient mechanics.
What you might notice: Shoulder “slipping” sensation, fatigue when doing long sets, uneven stroke power.
5. Scapular Dyskinesis
The shoulder blade (scapula) must move smoothly to allow the arm to move efficiently overhead. When the scapula is not stable (dyskinesis), the shoulder joint takes extra loads.
Clinical clue: Asymmetry in the shoulder blade during movement, difficulty holding proper body roll or stroke posture, fatigue of shoulder stabilisers.How can swimmers and coaches address/prevent these injuries?
Here are practical tips to help avoid shoulder problems — and to manage them early if they arise.
Monitor training load – Avoid large sudden increases in volume or intensity. Gradual progression is safer.
Technique check – Regularly review stroke mechanics: hand entry, catch, pull-through, recovery, body roll. Poor mechanics = more shoulder stress.
Strength and conditioning – Emphasise rotator cuff strength, scapular stabilisation, core and trunk control. A balanced dryland program helps.
Scapular control – Exercises like scapular retractions, stabiliser work, serratus anterior strengthening are helpful.
Flexibility / mobility – Ensure adequate range of motion in the shoulder, thoracic spine, and control of the shoulder blade.
Early recognition – If a swimmer reports shoulder soreness that’s lingering, catching, or increasing during training—address it early rather than ignore it.
Load modification – If pain occurs, reducing volume, avoiding aggravating sets, and cross-training can prevent escalation.
Multi-disciplinary approach – Work with coaches, swim technique experts, strength & conditioning and physical therapy together for best results.When to see a physical therapist?
If you're a swimmer and experiencing:Persistent shoulder pain (that doesn’t go away after rest)Loss of stroke power or speed related to the shoulderClicking, catching, or instability in the shoulderRecurring shoulder issues
…then it’s a good idea to have an evaluation by a physical therapist experienced with swimmers. At JSR we assess shoulder strength/motion, scapular control, and work with you and your coach to build a targeted plan.Shoulder injuries in swimmers are common but not inevitable. With smart training, good technique, strength & mobility work, and early attention to symptoms, most swimmers can perform and train without chronic shoulder pain.At JSR, we aim to help you stay strong, efficient and injury-free in the pool. If you’d like a shoulder screening, or want to discuss swim-specific shoulder rehab, we’d be glad to help.How to Tackle the Aging Knee: What to Know about Arthritic Knee Pain
As we get older, our knees take a lot of wear and tear. One of the most common culprits behind knee pain is Knee osteoarthritis (knee OA) — a form of arthritis that affects the cartilage, bones, and other structures of the knee joint. In this post we’ll walk through what it is, why it happens more with age, who is most affected, and what you can do (with your physical therapist!) to feel better and stay active.What is Arthritic Knee Pain?
Knee osteoarthritis happens when the protective cartilage in the knee gradually wears down. This leads to changes such as:Bones rubbing or bumping each other,The joint lining becoming inflamed,Possible bony outgrowths (osteophytes), andStiffness, swelling and pain in and around the knee.
This doesn’t happen overnight — it’s a slow process, often over many years. It becomes more likely as we age, especially if we’ve had prior knee injury, are carrying extra weight, or have certain structural knee alignment issues.Why Age Matters
Age is one of the biggest risk factors for knee OA. Here are some key statistics:Globally, the prevalence of knee OA in people aged 15 and over is about 16.0%, and for those aged 40 and over it rises to about 22.9%. PMCAccording to the World Health Organization, about 73% of people with osteoarthritis are older than 55 years, and around 60% are female. World Health OrganizationIn the U.S., about 9.3% of the population is diagnosed with symptomatic knee OA by age 60. PMCAmong adults aged 45-64 in the U.S., symptomatic knee OA affects roughly 7.8% of people; for those over age 65 it rises to about 15.6%. PMCThe annual incidence (new cases) of knee OA is highest in the 55-64 age group. Osteoarthritis Action Alliance+1
In simple terms: as you cross into your 50s and beyond, the risk of developing knee osteoarthritis goes up significantly. The wear-and-tear over years, combined with factors like previous injuries, activity level, body weight, and genetics, all add up.Who is Most Affected?
While knee OA can occur in younger adults — especially if they’ve had knee injuries or are obese — the “aging” population is more commonly impacted. Some patterns to note:Women are at higher risk than men in many studies. PMC+1People who are overweight or obese have a higher risk (because extra weight increases the load on knee joints). BioMed Central+1The average/median age of diagnosis of symptomatic knee OA in one U.S. study was about 55 years. PMCAlthough older age groups have higher percentage prevalence, because there are many people in the 45-64 age range, the number of people with knee OA in that age band is nearly as high as older groups. PMC
For a physical therapy practice, this means many patients in their 50s, 60s and older will likely start showing knee pain from arthritic changes — but they don’t have to just accept it.What Does Knee Arthritis Feel Like?
In the clinic you may see patients describing:Gradual onset knee pain (often worse after activity or long periods of standing)Stiffness in the morning or after sitting for a whileDifficulty going up or down stairsA “giving way” or instability feeling (due to weakened muscles or altered joint mechanics)Possible swelling, warmth, or a “grating” feeling inside the knee
Because the condition progresses slowly, patients may attribute the symptoms to “just getting older.” It’s important to recognize that — yes, age is a factor — but there are things we can do to slow progression and improve function.How Physical Therapy Can Help
1. Strengthening & Muscle Support
Stronger muscles around the knee (quadriceps, hamstrings, glutes) take pressure off the joint and help improve alignment and movement patterns.2. Improving Mobility & Joint Mechanics
Gentle motion, stretching, and activity modification help maintain joint mobility so the knee doesn’t lock up or worsen stiffness.3. Activity Guidance
We’ll help patients stay active (which actually helps cartilage health) while avoiding movements that overload the knee. Low-impact aerobic work, proper footwear, and safe stair/step mechanics all matter.4. Weight & Load Considerations
A study found that for every 5lbs of fat, the load on the knee joint increases by 4lbs. So by losing even just 10lbs, it takes roughly 40lbs of pressure off of the knee joint.5. Education & Pain Management
Teaching patients about proper biomechanics, pain-relieving strategies, and strategies to avoid worsening the joint helps them stay in control.Age Groups & What to Know:
Here’s a breakdown of age bands and what to watch for:40-49 years: Some early arthritic changes may begin. Prior knee injuries, high impact sports, obesity matter. Early intervention is beneficial.50-64 years: This is often the “sweet spot” for diagnosis of symptomatic knee OA. Pain may become more noticeable, especially with stairs, walking, prolonged standing.65 years and older: Higher prevalence of knee OA; however, because of other comorbidities (balance issues, bone health, other joints), tailored rehabilitation is critical to maintain independence and mobility.
Key Take-Home Messages
Arthritic knee pain is very common in older adults — age 55 and up is where we start to see the bulk of diagnoses.You’re not just “old and sore” — knee osteoarthritis is a real joint condition that responds to intervention.Physical therapy is not too late at any age — strengthening, mobility work, load management and activity guidance can improve quality of life.The earlier you engage (even if symptoms are mild), the better chance you have of slowing progression and maintaining an active lifestyle.Age matters as a risk factor, but individual risk also depends on weight, injury history, activity level, and muscle strength/conditioning.
And to the active adults who still want to train like they did when they were younger— the key is finding the right volume that works for you. I personally used to play soccer everyday. But as I have gotten older, and my own personal knee arthritis has started to set in, I found that two days a week of soccer was doable without flaring up my knees. I also strength train and stretch at least 2 days per week to ensure my joints are protected when I step on the field. Sometimes figuring out the “right”" amount of volume takes some trial and error, but it is definitely possible with smart choices and discipline. Maybe it’s as simple as running 3 miles instead of 4 because you notice at 3.5-4 miles your knees ache for days. And instead of running daily you can choose to run every other day and supplement biking for extra cardio. These are all decisions we can help you with so feel free to reach out with any questions! Average Return‑to‑Sport Times After ACL Surgery: What the Research Really Shows
When athletes injure their ACL (anterior cruciate ligament), one of the first questions is: "How long until I can play again?" The honest answer is: it depends – but we have excellent research to help guide expectations…
When athletes injure their ACL (anterior cruciate ligament), one of the first questions is: "How long until I can play again?" The honest answer is: it depends – but we have excellent research to help guide expectations.The ACL is one of the key stabilizing ligaments in the knee, helping control rotation and preventing the shin bone from sliding forward. It is most often torn during sudden cutting, pivoting, or landing movements — especially when the foot is planted and the knee twists inward. Non‑contact injuries (like a quick change of direction or awkward landing) make up the majority of ACL tears in field and court sports.Below is a current look at what return-to-sport timelines look like today:The "6‑Month" Myth vs. Reality
Years ago, many athletes were told that they could return as early as six months after ACL reconstruction. Today, we know that rushing back too soon significantly increases the risk of re‑injury.
Modern research shows that athletes who return before 9 months are up to 7 times more likely to tear their ACL again.Differences by Sport:
Sports involving jumping, cutting, and pivoting — such as soccer, basketball, lacrosse, football, and tennis — typically require 9–12+ months before a safe return.
Linear sports like running or cycling may allow earlier return, often between 6–9 months, depending on symptoms and strength recovery.Why "time alone" isn’t enough:
Return‑to‑sport decisions today are based on criteria, not just the calendar. Common clearance factors include:Quad and hamstring strength symmetry (90% or greater)Balance and landing mechanicsSingle‑leg hop testingConfidence and psychological readinessMovement quality in cutting/jumping
Psychological Readiness Matters Too
Research shows that fear of re‑injury is one of the most common reasons athletes delay returning to sport—even when physically cleared. Structured rehab that includes confidence‑building and sports‑specific progressions leads to better outcomes.Key Takeaways:
Most athletes safely return to sport between 9–12 months after ACL reconstruction.Returning before 9 months dramatically increases the risk of re‑injury.A full clearance is based on performance criteria, not just the date on the calendar.Strength, control, and confidence are just as important as ligament healing.
If you’re recovering from ACL surgery or working your way back to your sport, a physical therapist can guide every phase of your rehab and testing so you return not only faster — but safer.Research Sources:
Grindem et al. "Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction." British Journal of Sports Medicine, 2016.
Beischer et al. "Young athletes who return to sport before 9 months after ACL reconstruction have a higher risk of reinjury." American Journal of Sports Medicine, 2020.
Ardern et al. "2018 International Olympic Committee (IOC) consensus statement on return to sport after injury." British Journal of Sports Medicine, 2018.
Understanding Frozen Shoulder
Frozen shoulder, also called adhesive capsulitis, is a painful condition that limits motion in the shoulder joint. It occurs when the capsule of connective tissue surrounding the shoulder thickens and becomes tight...
Frozen shoulder, also called adhesive capsulitis, is a painful condition that limits motion in the shoulder joint. It occurs when the capsule of connective tissue surrounding the shoulder thickens and becomes tight. This reduces the smooth gliding movement of the joint and makes even simple daily activities difficult, such as reaching overhead or behind the back.This condition affects an estimated two to five percent of the general population. It is more common in adults between the ages of forty and sixty and is seen more often in women than in men. People with diabetes are at a much higher risk. Research shows that as many as twenty percent of people with diabetes will develop frozen shoulder at some point.Frozen shoulder usually develops in stages and may take many months to improve.How Long Does Frozen Shoulder Last
Frozen shoulder is temporary. The process usually lasts from one to three years, though many people begin feeling better much sooner once motion improves and the irritation settles. With consistent therapy and proper pacing, the shoulder often regains strength and mobility far earlier than the complete timeline suggests.Common symptoms include:
Deep aching pain in the shoulder
Stiffness and loss of motionDifficulty sleeping because of shoulder discomfortWeakness due to pain and guarding
The pain is often constant and can worsen at night. Over time, the joint becomes more restricted which limits normal movement during daily tasks. These symptoms are frustrating, but they are reversible and can respond well to guided care.The Three Phases of Frozen Shoulder
Frozen shoulder develops in a predictable pattern. Understanding the stages helps patients stay encouraged during treatment.Freezing Phase: Pain begins gradually and motion becomes limited. The shoulder feels stiff and irritated. This is when calming the joint is most important.Frozen Phase: Pain often begins to lessen, while stiffness remains the main concern. Many people begin to feel small gains in comfort during this period.Thawing Phase: Movement steadily improves and the shoulder becomes more flexible. This is the stage where patients often feel major progress and return to confident use of the arm.Why Hyperirritability Matters in Physical Therapy:
Many patients with frozen shoulder experience what therapists call a hyperirritable shoulder. This means the tissues react strongly even to gentle stretching or light pressure. Because of this, pushing too hard can increase pain and slow progress.
A thoughtful approach to physical therapy is important. Treatment often focuses first on calming the irritated tissues through gentle movement, soft tissue work, and pain control strategies. Only after the irritation settles can more aggressive stretching be introduced. Physical therapy that accounts for tissue irritability of the shoulder responds better and recovery tends to move forward more smoothly.It is very important to not just push through pain. If you are noticing that your shoulder pain and stiffness is worse that night or the next day following stretching/exercises, than you need to go lighter with your program. Non Surgical Treatment Options:
Most people improve with non surgical care. These treatments includePhysical therapy to restore motion, strength, and joint mobilityTargeted stretching taught in a gradual and safe mannerHeat or cold for pain reliefJoint mobilization performed gently by a licensed therapistAnti inflammatory medication when recommended by a medical providerCorticosteroid injections in some cases to calm inflammation
With committed participation many patients see significant improvement in function over time without the need for an operation.Surgical Treatment Options:
If pain and stiffness remain severe and do not improve after several months of therapy, a physician may recommend a surgical option. The two most common procedures areManipulation under anesthesia, where the doctor gently moves the shoulder to loosen the tight capsuleArthroscopic capsular release, where tight tissue is carefully trimmed to restore motion
Even after surgery, physical therapy remains an important part of recovery to maintain the gains in mobility and to retrain healthy shoulder movement.The Outlook:
The outlook for frozen shoulder is encouraging. The body is built to heal this condition and the great majority of people regain comfortable function. With patience, proper pacing, and skilled therapy, daily activities become easier and confidence in the shoulder steadily returns. Progress sometimes feels slow early on, but it builds momentum as the shoulder moves from stiffness toward freedom of motion.Why Ankle Sprains Are the Most Common Sports Injury — and How to Recover Stronger
Whether you’re playing basketball on the court, sprinting down a soccer field, or diving for a volleyball save — your ankles are doing a lot more work than you think. In fact, ankle sprains are the single most common injury in sports, accounting for up to 40% of all athletic injuries worldwide.
Recent studies show that athletes in court sports like basketball and volleyball face the highest risk — often more than 5 sprains for every 1,000 games or practices. Field sports such as soccer and football aren’t far behind, with frequent twists, tackles, and uneven turf contributing to steady injury rates year after year.
Once you sprain an ankle, your odds of doing it again increase. Research suggests that nearly 1 in 5 athletes will experience recurrent sprains or develop chronic ankle instability, leading to ongoing weakness, swelling, or “giving way.”
But here’s the good news: understanding which sports carry the highest risk helps athletes, coaches, and clinicians focus on prevention — from strength and balance training to proper taping/footwear.What These Numbers Mean for You
The chart above isn’t just about numbers — it’s about how your sport stacks up in ankle risk and what that means for keeping you on your feet.Court sports (like basketball and volleyball) lead the pack for ankle sprains because of the constant jumping, cutting, and landing on other players’ feet. Quick direction changes and rebounds make these sports a perfect storm for rolled ankles.Field sports (like soccer, football, and rugby) cause more contact-related ankle injuries — think awkward tackles, slippery grass, and high-velocity collisions. These injuries often involve the syndesmosis (“high ankle”) and can sideline athletes longer.Repetition matters: The more you play, the higher your exposure risk. That’s why professionals and year-round athletes report higher rates than casual players.Prevention pays off: Studies consistently show that ankle braces, taping, and neuromuscular training can cut sprain rates by 40–50%.Rehab isn’t optional: Once you’ve sprained an ankle, skipping rehab doubles your chances of another injury — and long-term instability can linger for years.
Bottom line: No matter your sport, ankle strength and balance training aren’t just accessories — they’re your best defense against the most common injury in athletics.
Every ankle sprain tells a story — but at our clinic, we make sure it doesn’t become a recurring chapter. While most people think a sprain just needs rest and time, research shows that without proper rehab, up to 70% of athletes develop lingering weakness or instability. That’s where physical therapy makes the difference.At our facility, recovery isn’t a one-size-fits-all process. We combine evidence-based rehab with sport-specific retraining to restore balance, strength, and movement confidence — so you can return not just to play, but to peak performance.How We Address Ankle Sprains In Physical Therapy:
Early Phase: Calm the Injury, Set the Foundation
In the first stage, our priority is to reduce swelling, relieve pain, and restore gentle motion. We also strengthen the joints and muscles above the ankle — the hips, knees, and core — to keep your body balanced during recovery.
We introduce light neuromuscular and proprioceptive training early to keep your ankle connected to your brain’s balance system.Treatments that accelerate this phase include:MyACT Piezowave therapy (shockwave treatment) to boost circulation and healing.Targeted massage and voodoo band compression to reduce swelling and stiffness.Dry needling to relieve pain and improve muscle activation.24/7 compression sleeve use to manage swelling and promote recovery.
Mid Phase: Rebuild Strength and Control
Once swelling subsides and motion returns, we shift focus toward building ankle strength, balance, and coordination.
This stage bridges basic movement and athletic function — restoring your ankle’s ability to stabilize under everyday and athletic demands.Our focus:Progress range of motion and resistance training.Introduce balance and proprioception drills on stable and unstable surfaces.Continue managing any residual swelling to ensure smooth progress.
End Stage: Return to Power and Performance
The final stage is where athletes regain their explosiveness, agility, and sport-specific readiness.
We integrate plyometrics, cutting, and directional drills that mimic your sport’s real-world challenges — basketball jumps, soccer pivots, football sprints, and more.The goal: Build a resilient ankle capable of handling rapid movements, unpredictable landings, and high-impact demands — without fear or instability.Ready to Start Your Recovery?
Don’t let an ankle sprain keep you on the sidelines longer than it should. Whether you rolled your ankle last week or have been dealing with chronic instability for years, the right physical therapy approach can make all the difference.Schedule your ankle recovery evaluation today and take the first step toward getting back to the sport you love — stronger than before.Building Better Athletes: A Smarter Path Back to Sport
At J Sports Rehabilitation (JSR), we believe every injury is an opportunity to rebuild and come back stronger. Our mission is to bridge the gap between injury rehabilitation and full return to sport or activity through a collaborative, athlete-centered approach….
At J Sports Rehabilitation (JSR), we believe that every setback is an opportunity for growth. When an athlete is injured, it’s not just about recovery — it’s a chance to rebuild, re-establish proper movement patterns, and strengthen the body as a whole. Injury can be the beginning of a smarter, stronger return to sport.
When professional athletes get hurt, they’re supported by a full team — doctors, physical therapists, athletic trainers, and performance coaches — all working together to create the best possible outcome. At JSR, we believe this level of coordinated care shouldn’t be reserved for elite athletes.
Our mission is to bridge the gap between injury rehabilitation and full return to sport or daily activity. You don’t need to play professionally to deserve a team dedicated to your recovery — and your success.Comprehensive Sports Rehabilitation for Every Athlete
We work with adults and young athletes recovering from knee, hip, foot/ankle, shoulder, and back surgeries. Our goal is to collaborate seamlessly with your medical providers and strength and conditioning coaches to ensure a smooth, safe, and effective recovery.
Whether you’re returning from an ACL reconstruction, rotator cuff repair, hip labral surgery, or a muscle strain, our team helps you progress confidently back to the sport or activity you love. Every plan is customized to your goals — from rebuilding strength and stability to restoring speed, power, and confidence in movement.The Return to Sport Difference
Our Return to Sport Program was designed to give every athlete access to the same high-quality, team-based care used at the professional level.In the early phases of recovery, your physical therapist leads the process, focusing on healing, mobility, and proper movement patterns. As you advance, we begin to integrate modified strength training with your coach to prepare you for full performance.For example:If you’re recovering from an ACL injury, your strength coach can guide upper-body development during the early recovery phase.If you’re rehabbing a shoulder injury, your coach can focus on lower-body strength to maintain balance and progress.
This collaborative model ensures your entire body continues to improve — not just the injured area.A Team Approach to Athletic Recovery
At JSR, our team communicates across disciplines — sharing updates, insights, and progress notes to make sure your rehabilitation, strength training, and performance goals align perfectly. The result is a seamless transition from rehab to training to competition.The goal is simple: to help you return stronger, more balanced, and more resilient than before.In partnership with SPECTRUM Performance and Competitor Performance Academy, we don’t just help you recover — we help you build a better athlete.Understanding Headaches: Causes, Types, and Relief Strategies
Headaches are the most common pain disorder worldwide, affecting roughly 66% of the global population. The International Headache Society classifies headaches into several categories:Tension-type headachesCervicogenic headachesMigraine and cluster headachesSecondary headaches resulting from underlying conditions (e.g., fever, infection, sinus issues, or tumors)Cranial neuralgias, facial pain, and other headache syndromes
Tension-Type Headaches
Tension-type headaches are the most common form of headache in adults, with studies suggesting that 30–80% of U.S. adults experience them. These headaches often result from stress, poor posture, fatigue, jaw or neck pain, or dysfunctional breathing patterns.People often describe the pain as a dull ache or tight, band-like pressure around the head — particularly at the temples, forehead, or the back of the neck. The discomfort can last anywhere from 30 minutes to several days and usually affects both sides of the head, although it may occasionally occur on one side.Anatomically, this pain occurs because the neck muscles attach to the cervical spine and skull. When these muscles tighten or spasm, they can “tug” on the skull and create tension that radiates into different regions of the head. Depending on which muscles are involved, pain may be felt at the base of the skull, across the forehead, or above the eyes.Common Muscles That Contribute to Tension Headaches
Upper TrapeziusSternocleidomastoidLevator ScapulaeSuboccipitalsScalenes
These muscles, when tight or overused, can refer pain into the head and mimic classic headache symptoms.
Managing Tension Headaches
Over-the-counter medications such as Tylenol, Advil, Motrin, or Aleve can help relieve symptoms, but it’s important to consult your doctor before use. Always take the lowest effective dose, as overuse can sometimes lead to rebound headaches — a worsening cycle of pain triggered by frequent medication use.Cervicogenic Headaches
Unlike tension headaches, cervicogenic headaches stem from dysfunction in the upper three cervical spine segments (facet or zygapophyseal joints). Nerves originating in the cervical spine provide sensory and motor information to the head and neck, and irritation of these nerves can produce referred pain that mimics a headache.Common Identifiers of Cervicogenic Headaches:
Pain primarily on one side of the head (though both sides can be affected)Restricted neck movement or stiffnessPain triggered by neck movement or awkward posturesPain reproduced by pressure at the base of the skull or upper cervical spineAccompanying same-sided neck, shoulder, or arm pain
Treatment and Outlook
Research shows that neck-specific exercises — particularly low-intensity endurance training — and spinal mobilization can be effective both in the short and long term for managing cervicogenic headaches.It’s also important to note that not all headaches share the same cause. Some result from dehydration, lack of sleep, or underlying medical issues. Identifying the root cause is the first step toward effective relief — and many cases can be managed without heavy reliance on medication.In some instances, a local anesthetic injection may be required for pain relief, but this is typically reserved for more severe or persistent cases. Physical therapists can play a crucial role in addressing both tension-type and cervicogenic headaches through posture correction, strengthening, and manual therapy. When in doubt, consult a neurologist or primary care physician to help determine the underlying source of your headache.Treatment Strategies:
1. Posture Correction & Mobility Exercises
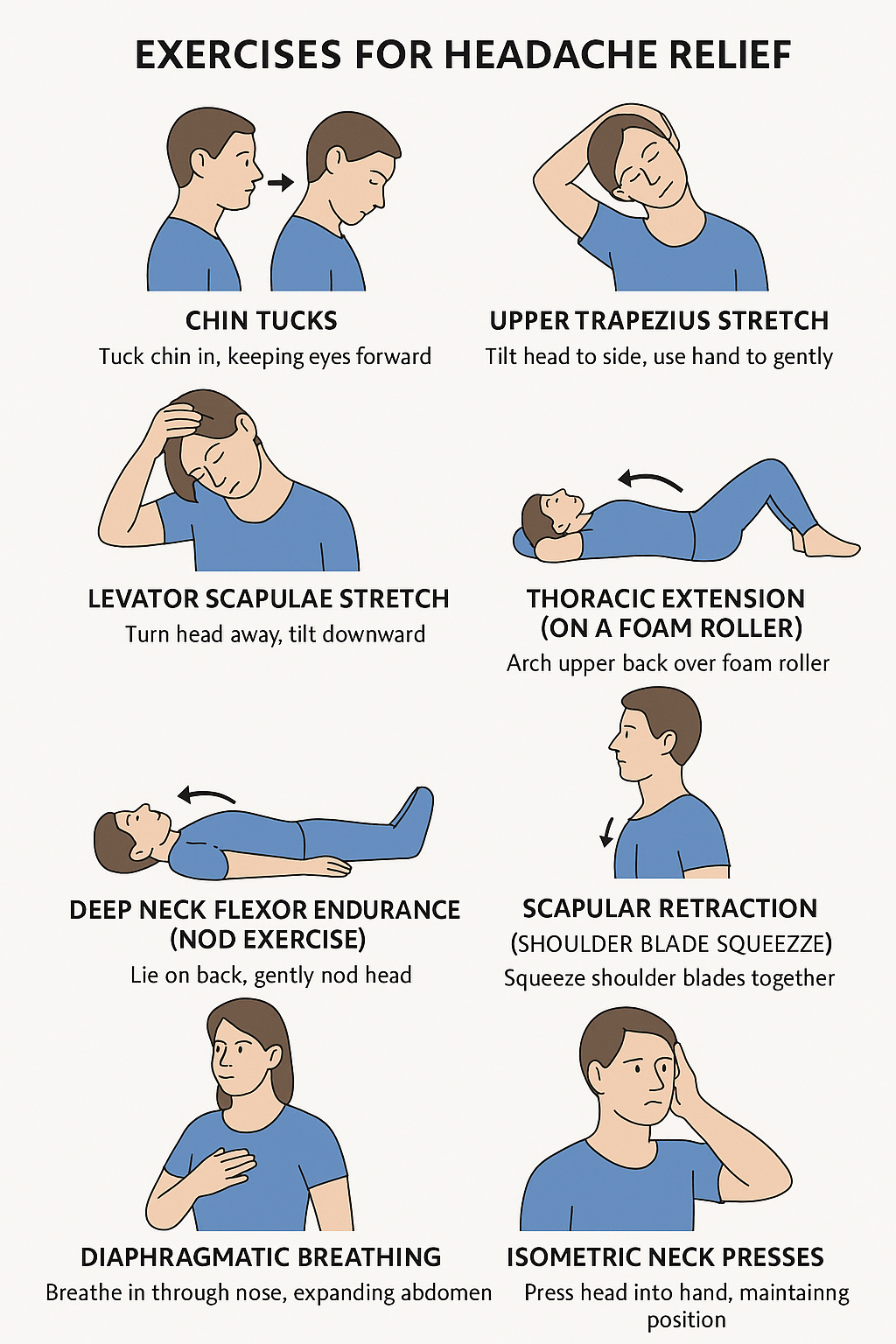
These target stiffness and poor alignment — common triggers for both tension-type and cervicogenic headaches.Chin Tucks
How: Sit or stand tall. Gently draw your chin straight back (as if making a double chin), keeping your eyes level.Hold: 5 secondsReps: 10–15Goal: Strengthen deep neck flexors and counteract forward-head posture.
Upper Trapezius Stretch
How: Sit tall. Gently tilt your head to one side (ear toward shoulder). Use your hand to lightly increase the stretch.Hold: 20–30 seconds each sideReps: 2–3 per sideGoal: Reduce tightness in the upper trapezius muscles.
Levator Scapulae Stretch
How: Sit tall. Turn your head 45° to one side, then look down toward your armpit. Use your hand to apply gentle pressure on the back of your head.Hold: 20–30 seconds each sideReps: 2–3 per sideGoal: Decrease neck base and shoulder tension.
Thoracic Extension (on a Foam Roller)
How: Lie with a foam roller under your upper back, knees bent. Support your head and gently arch backward over the roller.Hold: 2–3 secondsReps: 10–12Goal: Improve upper-back mobility and reduce strain on the neck.
2. Neck Strengthening & Endurance Training
These build stability in deep neck muscles that often weaken due to poor posture or prolonged screen time.Deep Neck Flexor Endurance (Nod Exercise)
How: Lie on your back with knees bent. Gently nod your head (“yes” motion) without lifting it off the floor.Hold: 5–10 secondsReps: 10–12Goal: Strengthen deep cervical flexors — crucial for posture and neck support.
Scapular Retraction (Shoulder Blade Squeeze)
How: Sit or stand tall. Gently squeeze your shoulder blades together and down (avoid shrugging).Hold: 5 secondsReps: 10–15Goal: Strengthen mid-back muscles that support the neck.
Isometric Neck Presses
How: Press your head gently into your hand (forward, backward, side to side) without actual movement.Hold: 5 seconds each directionReps: 5–10 each wayGoal: Build neck stability and reduce muscular fatigue.
3. Breathing & Relaxation Techniques
Dysfunctional breathing and stress can amplify headache frequency and intensity.Diaphragmatic Breathing
How: Sit or lie comfortably. Place one hand on your belly and one on your chest. Inhale deeply through your nose so your belly rises, then exhale slowly through your mouth.Duration: 2–5 minutesGoal: Reduce muscle tension and activate relaxation responses.
4. Daily Habit Fixes
Simple lifestyle adjustments can make these exercises even more effective:Take movement breaks every 30–45 minutes during desk work.Keep your monitor at eye level to reduce neck strain.Stay hydrated and get adequate sleep.Consider gentle yoga or Pilates to maintain flexibility and posture control.
Understanding Hamstring Injuries in Sports: How Common Are They—and What You Can Do
Hamstring injuries are one of the most common complaints among athletes—especially in sports involving sprinting, kicking, or sudden stops and starts. If you’ve ever pulled up with a tight back thigh or heard the dreaded “pop,” you know just how disruptive these injuries can be. In this post, we’ll look at what the research says about how often hamstring injuries happen, who’s at risk, and what physical therapy can do to prevent and recover from them.
Hamstring injuries are one of the most common complaints among athletes—especially in sports involving sprinting, kicking, or sudden stops and starts. If you’ve ever pulled up with a tight back thigh or heard the dreaded “pop,” you know just how disruptive these injuries can be. In this post, we’ll look at what the research says about how often hamstring injuries happen, who’s at risk, and what physical therapy can do to prevent and recover from them.What Are Hamstring Injuries?
The hamstrings are a group of muscles and tendons at the back of the thigh. Injuries range from mild strains (small tears) to more serious ruptures or tendon injuries. Some are acute (sudden) while others develop over time or recur.How Common Are They?
Here are some key statistics from recent studies:Incidence in field‑based team sportsAbout 0.81 hamstring injuries per 1,000 exposure hours (training + matches) in sports like soccer, rugby, field hockey, Gaelic football, Australian football. PubMedProportion of all sports injuriesHamstring injuries make up ~10% of all injuries in those same sports. PubMedPrevalence over a season (~9 months)Around 13% of athletes will suffer a hamstring injury during a typical 9‑month season in field‑based team sports. PubMedChange over time (professional male soccer) In one 21‑season study in European male professional soccer: hamstring injuries went from accounting for ~12% of all injuries in early seasons to 24% in more recent seasons. The number of days players miss from these injuries also doubled. PubMed+1
Risk Factors: Who’s More Likely to Get Them?
During matches vs training: Hamstring injuries are much more likely during matches than training. In one review, match injury incidence was ~9.4‑fold higher than training. PubMedAge: Risk increases with age; older athletes have higher rates of hamstring injury. PubMedSurface type: Injuries are more common on natural grass vs artificial turf. PubMedPrevious injury: Athletes who have had hamstring injuries before are at greater risk of recurrence. JOSPT+2JOSPT+2
Why Are Hamstring Injuries Getting More Common?
The studies suggest a few trends:Increasing match intensity and schedules (more games, less rest). PubMed+2JOSPT+2Greater demands during training sessions. PubMed+1Possibly more awareness/reporting and better diagnostic tools, which may increase recorded incidence.In professional soccer, the “burden” (how many days missed, how long players are out) of hamstring injuries has increased over time. PubMed+1
How Physical Therapy Helps: Prevention & Recovery
Here’s how a physical therapist can help reduce risk and get you back in the game.Screening & AssessmentAssess strength, flexibility, muscle imbalances.Examine movement patterns, running or sprint mechanics.
Targeted Strength TrainingEccentric training (lengthening under load) is especially effective for hamstrings.Balance between hamstrings and quadriceps/groin muscles.
Flexibility & MobilityRegular hamstring stretches and dynamic warm‑ups.Also hip flexor and glute work to ensure pelvis positions are optimal.
Load ManagementGradually increasing training intensity.Ensuring adequate rest between high‑intensity efforts.
Neuromuscular Control & TechniqueDrills for proper technique in sprinting, cutting, stopping.Core stability, pelvic control, coordination.
Return‑to‑Sport PlanningGradual return with progressive demands.Monitoring for signs of fatigue or tightness.Ensuring full recovery before resuming sprinting or cutting loads.
Takeaway
Hamstring injuries are frequent, costly, and appear to be increasing in both number and severity—especially in sports with high demands like sprinting, football/soccer, rugby, etc. But they’re not inevitable. With careful prevention, good rehab, and smart training loads, many athletes can reduce their risk and recover fully if injury does happen.Let us know if you have any questions. We are happy to help!Shoulder Instability: Do you have Multidirectional Instability?
Do you commonly feel like your shoulder is unstable or “pops” in and out of place? If you do then you may have something called Multidirectional Instability (MDI).
Do you commonly feel like your shoulder is unstable or “pops” in and out of place? If you do then you may have something called Multidirectional Instability (MDI).
MDI is defined as laxity in the shoulder joint in multiple directions.MDI is either caused by a traumatic or atraumatic mechanism. That means the individual either had: 1. A traumatic incident like a fall, which leads to dislocation of the shoulder joint. This dislocation ultimately leads to residual laxity in the shoulder OR 2. They are a generally hypermobile individual, perform repeated overhead movements (such as with volleyball, baseball, weight lifting, etc), and have a history of subluxationsWhat is the Difference between a Subluxation and Dislocation?A Dislocation is considered a displacement of the bone from its natural position in the joint. The humeral head completely comes out of place and may require medical intervention to return the bone back into place.A Subluxation is a partial dislocation of the joint. Typically the shoulder will feel like it pops out of place but then will quickly pop back into place.Common MDI Presentation:
<35 years of ageTypically uses words like “double jointed” or “always been flexible” to describe themselvesMultiple episodes of subluxationPain or feeling of instability typically at the end range of motionHistory of participating in overhead sports (MDI may be related to repeated microtrauma)
The good news is nonsurgical, conservative care is frequently recommended for MDI. The bad news is that these individuals will need to be diligent with a strengthening program to reduce the risk of subluxations in the future. I have seen many clients with MDI and the key is to strengthen the rotator cuff, scapulo-thoracic complex, core and hips. Addressing Range of Motion should NOT be the focus for these individuals. You do not want to create further instability by stretching the joint. Trigger point release is okay however to alleviate pain caused by overuse of the muscles associated with instability. The exercises below are a great way to start addressing MDI. Let me know if you have further questions at rachel@jsportsrehab.com!
Band Resisted Shoulder External Rotation (Bilateral):
Band Resisted Internal Rotation:
Band Resisted External Rotation:
Wall Walks:
Supine Arm Bar:
Anterior Hip Pain: Do you have Femoroacetabular Impingement (FAI)?
A recent case: A 19 year old female soccer player presented to therapy with pain into the front of her right hip and groin. She is a right footed soccer player and reported a pinch-like pain into the front of her hip as her leg traveled across her body when shooting. She also felt pain when hugging her knee to her chest and an aching pain into the hip after sitting for a few hours. She kept playing through the pain and reported the pain just seemed to get worse and worse. Clinical testing suggested she had hip impingement but Imaging from a physician officially diagnosed her with a pincer type of impingement. What is FAI?
An Overgrowth of either the femoral head or the acetabulum (hip socket). It is defined as motion or position related pain in the hip or groin with possible clicking, catching, locking, stiffness, giving way, and decreased range of motion.2 Types of FAI:1. CAM: Overgrowth of Bone at the Femoral Head2. Pincer: Overgrowth of Bone at the AcetabulumCAM Impingement is more commonly seen in males in their 20s vs Pincer impingement is more commonly seen in females in their 30s and 40s.Both types of impingement can feel like a pinch. That is because there is an overgrowth of bone in the hip joint. The head of the femur and the hip socket basically bump into each other during any motions where you bring your hip up to your chest. This “bumping” or frictioning of bone on bone is not only painful, but can lead to damaging the labrum over time. The labrum is what cushions the femoral head within the socket. Damage to the labrum can potentially lead to longer recovery times or even surgery. Symptoms:
Pain or aching (usually located at the inner hip, or groin area), usually after walking, or prolonged sittingA locking, clicking or catching sensation within the jointPain bringing your hip up towards your chest and and across the body towards the opposite shoulder
How to Diagnose:
Clinical Testing: FADIR and FABERRange of Motion: Limitations in hip Internal rotation and flexionImaging: X rays, Magnetic Resonance Athrography (MRA), or CT scan
Treatment:
Conservative Treatment: Physical Therapy/Activity Modification: Avoid activities that cause pinching/pain– Activity Modification: Avoid activities that cause pinching/pain– Rehab Focus: Address hip strength, hip stability, neuromuscular control, range of motion, and movement mechanicsSurgical Intervention: Hip arthroscopy or open surgery: recovery time 4-6 months
Sports you are more likely to see impingement in:
Soccer, martial arts, ballet, cycling, rowing, golf, tennis, football, hockey, baseball, lacrosse, rugby, and deep squatting activities such as powerlifting.
Interesting Fact:
CAM impingement is common in male soccer players, with 60-75% of adult male soccer players found to have this type of impingement. This number is high especially when considering the prevalence of CAM in the general person is only roughly 17-20%.
Exercise Ideas:
Hip Flexor Release: https://www.youtube.com/watch?v=f13QETYZQMgQuadriceps Stretch:Couch Stretch: https://www.youtube.com/watch?v=tABeNRBDf30Bridge: https://www.youtube.com/watch?v=gYVVdmARLuUClamshell: https://www.youtube.com/watch?v=2OhR279AWNYSide Plank: https://www.youtube.com/watch?v=TPp92f8HlG0Single Leg Bird Dog: https://www.youtube.com/watch?v=GlutdS3NdXQThoracic Mobility: Important for Every Sport and Movement in Life!
Do you have low back pain, shoulder pain, or neck pain? Do you want to improve your golf swing, overhead serve in volleyball, hitting power in baseball and softball, or pitching velocity?
Do you have low back pain, shoulder pain, or neck pain? Do you want to improve your golf swing, overhead serve in volleyball, hitting power in baseball and softball, or pitching velocity?
As a physical therapist, the thoracic spine is one of first areas I treat. Whenever you lift your arm overhead, throw a ball, swing a golf club, or even look up at a book on a high shelf, your thoracic spine is moving.Try this: relax your upper back and shoulders and get really slouchy in your chair. Now try looking up at the ceiling. Then try lifting your arm overhead… Hard right? Now sit up nice and tall in your chair and perform the same two movements. Should be much easier, more comfortable, and you should be able to get more range of motion in your neck and shoulder. I know this is a very extreme example but imagine how much even a little bit of thoracic spine stiffness can affect how you get your arms overhead to spike a ball in volleyball or throw a baseball.Common problems associated with poor thoracic mobility include shoulder impingement/pain, low back pain, and neck pain. There are other factors that can contribute to these same issues but, in this article, we are going to focus on the thoracic spine as the root of the problem. When the thoracic spine doesn’t move, your low back starts to pick up the slack. Instead of getting normal extension through your thoracic spine you end up hyperextending through your lumbar spine. This repetitive lumbar hyperextension leads to pinching posteriorly of the bones in your low back, thus resulting in pain. The same issues can happen at your neck.When you lift your arm overhead and you cannot extend in the thoracic spine, what will typically happen is your humerus will jam up against the acromion (See picture below). Having this bone to bone contact overtime can lead to pain. This same issue can also lead to rotator cuff muscle microtears because the rotator cuff muscle sits right underneath the acromion, and the friction of the constant bone to bone contact can lead to fraying of the muscle underneath.From a performance perspective in overhead athletes or overhead lifting (push press, push jerk, overhead squat), more force can be generated and more weight can be lifted when you have the range of motion to complete the movement. To properly engage your shoulder blade muscles and have your shoulder blade sit properly on the ribcage, you need full range of motion of the shoulder joint and thoracic spine. If not, like we mentioned before, your shoulder blades will sit forward on your ribcage (like with bad slouching posture) and your shoulder blade muscles won’t be able to engage properly. The better your shoulder blade muscle strength and stability are, the more power you can generate and the more weight you can lift overhead.Imagine swinging a baseball bat if you can’t rotate your thoracic spine. With this limitation the force you can produce when you hit the ball will be considerably less as compared to being able to rotate your spine fully.Here are some exercises you can do on your own to address this area of the body:7 Common Reasons Why You Have Shoulder Pain
Shoulder pain is one of my favorite issues to treat. For me, shoulder pain is easy to treat. Why? Because there are a lot of commonalities among individuals that come to me with shoulder pain, no matter what type of shoulder pain it is. No, not everyone with shoulder pain will have the same exact 3 or 4 problems; which is why an extensive examination is necessary before I start treating someone. However, I still find that most of my shoulder pain patients have a few things in common. Listed below are the top 7 dysfunctions I see in my shoulder patients:1. Restricted pectoralis minor/major flexibilityYou will notice difficulty reaching behind your back
2. Restricted latissimus dorsi flexibilityYou will notice difficulty raising your arm to your ear
3. Trigger points (muscle knots) that refer pain into the shoulderIf you apply deep pressure to certain muscles, you will feel tender points that refer pain elsewhere (especially common with the rotator cuff muscles that sit on top of your shoulder blade)
4. Forward head and shoulder postureMost people have sitting jobs and tend to sit with slouchy posture
5. Overactivation of the upper trapezius musclesYou will notice you constantly shrug your shoulders up when lifting your arm overhead
6. Weak scapular retractors, core, and rotator cuff muscles
7. Poor motor controlYou have the range of motion but your body doesn’t engage the right muscles at the right time appropriately to perform a specific movement
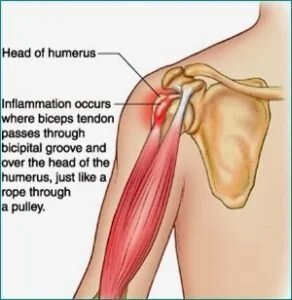
Next I want to talk about some common diagnoses I hear when a patient walks into my facility.Pain in the biceps or the front of the shoulder: A lot of times people come in with pain in the front of the shoulder and have been told they have a biceps tendonitis/tendonapathy. If you hear this diagnosis it means your biceps tendon has taken on extra work because your rotator cuff muscles, your scapular stabilizers and your core are slacking on the job. Other common issues found with this diagnosis include: restricted thoracic mobility, and slouchy forward head and shoulder posture, tight pectoralis minor/major muscles, and potentially tight latissimus dorsi muscles.
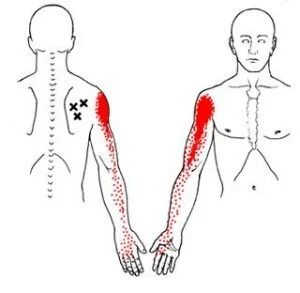
Pain that travels from the top of your shoulder down your arm an inch or two? This sensation is commonly due to what we call active trigger points (inflamed muscle knots). Your rotator cuff muscles, which sit on top of the shoulder blade, can develop trigger points that can refer pain into the shoulder and, at times, down the arm. Performing soft tissue massage using the lacrosse ball on tender or tight spots will help calm down the muscle and reduce the feeling of pain traveling into your shoulder.
Pain at the top of the shoulder joint and pain with raising your arm to end range overhead: This type of pain is typically given the diagnosis of shoulder impingement/ bursitis. This occurs because the humerus (arm bone) basically jams into the top of the shoulder joint whenever you raise your shoulder overhead. These people typically have bad forward head and shoulder posture. This diagnosis is either due to excessive shoulder mobility, or it is due to tight shoulder musculature (pectoralis minor/major, lats, rotator cuff muscles), overuse of the upper trapezius muscles, restricted thoracic mobility, or the inability to use your back, shoulder blade and core muscles efficiently. The latter option I tend to see more often.
Shoulder pain that is associated with weakness and, at times, the inability to lift your arm overhead: This injury can result from a traumatic fall or gradual wear and tear of the muscle with overhead activity. Common issues I see with this diagnosis include: forward head and shoulder posture, restricted thoracic mobility, tight shoulder musculature (pectoralis minor/major, latts, Rotator Cuff muscles), overuse of the upper trapezius muscles, and you are not using your back, shoulder blade and core muscles efficiently.
Notice a trend with some of the different diagnoses?.. It may seem like I am repeating myself a lot but most shoulder diagnoses stem from the same problems (excluding traumatic shoulder injuries of course). If you have shoulder pain and are reading this article then attacking the 7 problems I have listed above is a good place to start.Patellar Tendinopathy (Jumpers Knee):
Have you ever had pain in the front of the knee with jumping, cutting, running, or kicking? I personally have and it stinks. I played soccer growing up so the feeling of a sharp jolt to the front of the knee is not something foreign to me. To those of you experiencing the same sharp pain to the front of the knee, you will know that it feels as if you are running or jumping on eggshells.
What Is It and How Do You Treat It?
Have you ever had pain in the front of the knee with jumping, cutting, running, or kicking? I personally have and it stinks. I played soccer growing up so the feeling of a sharp jolt to the front of the knee is not something foreign to me. To those of you experiencing the same sharp pain to the front of the knee, you will know that it feels as if you are running or jumping on eggshells. You want to be explosive but you feel like if you bend your knees too much to really generate power or to absorb a landing, the sharp jolt is just waiting for you not far behind. I experienced this pain as a soccer player but it affects many other sports such as basketball, volleyball, tennis, track and field, football and the recreational runner. Athletes between the ages of 15 to 30 are primarily affected, with men more commonly affected than women. By definition, patellar tendinopathy (Jumper’s knee) is an overuse injury thought to be caused by excessive or repetitive forces applied to the patellar tendon. Signs and Symptoms of Patellar Tendinopathy:
Anterior knee pain over the patella tendonTenderness at the inferior pole of the patellar tendonPain made worse with jumping, landing, cutting/pivoting, or running activitiesPain with stairs, squatting, and at times prolonged sittingOnset of pain is usually gradual and commonly related to an increase in sport activityThe feeling of stiffness in the patellar tendon in the morningIncreased thickness of the patellar tendon compared to the opposite side
What is the Function of the Patellar Tendon?
The patellar tendon attaches directly from the tibial tuberosity to the inferior tip of the patella (knee cap). The quadriceps muscle attaches into the superior tip of the patella, thus transmits forces through the patellar tendon based on the common attachment into the patella. Therefore, any tightness or weakness in the quadriceps pulls on the patellar tendon. The patellar tendon also functions in the storage and release of energy when you jump, run, cut or pivot. This means there is a lot of load that has to transfer through the patellar tendon so overtraining, insufficient rest, faulty movement patterns, mobility impairments, and hip, core and foot weakness can contribute to the development of patellar tendinopathy.Common Impairments Found in Individuals with Patellar Tendinopathy:
Hip Abductor and Hip External Rotator WeaknessAltered Hip and Knee Movement Patterns upon Landing (Poor Movement Quality)Excessive or Restricted Hip and Ankle MobilityLook for reduced dorsiflexion, quadriceps or hamstring tightness, hip Internal rotation mobility, increased varus foot alignment, etc.
Quadriceps WeaknessExcessive Foot Pronation: foot collapses inward upon landing which causes knee valgus (knee collapse inward) as well as the femur to then internally rotate excessively
Rehabilitation Focus:
Eccentric Quadriceps StrengtheningQuadriceps and Hamstring FlexibilityHip Abduction and External Rotation StrengtheningMovement Competency–May require Cueing from a Rehab Professional or Qualified Strength Coach to address running, cutting, and jumping mechanicsFoot and Ankle StrengtheningAnkle Dorsiflexion Range of Motion
Exercise Ideas:
Here are some exercise ideas to get you started but it is always helpful to seek help from a medical professional.Quadriceps Flexibility:Couch Stretch: https://www.youtube.com/watch?v=tABeNRBDf30
Hip External Rotation Strengthening:Clamshell: https://www.youtube.com/watch?v=2OhR279AWNYFire Hydrant (can add band around knees to increase difficulty): https://www.youtube.com/watch?v=0Vk6BrtikL8Side Plank with Clamshell: https://www.youtube.com/watch?v=82tKGsLrADY
Hip Abduction Strengthening:Sidelying Hip Abduction: https://www.youtube.com/watch?v=Ku6QkDJqdwYSide Plank: https://www.youtube.com/watch?v=TPp92f8HlG0
Ankle Dorsiflexion:Mobilization with Movement: Long Sitting Position with Mobility Band: https://www.youtube.com/watch?v=sBCMIaIkP8cWall Stretch: https://www.youtube.com/watch?v=9QRVlaw9QWM
References:
Malliaras, P., Cook, J., Purdam, C. and Rio, E. (2015). Patellar Tendinopathy: Clinical Diagnosis, Load Management, and Advice for Challenging Case Presentations. Journal of Orthopaedic & Sports Physical Therapy, 45(11), pp.887-898.
Mendonça, Luciana D., et al. “Association of Hip and Foot Factors With Patellar Tendinopathy (Jumper’s Knee) in Athletes.” Journal of Orthopaedic & Sports Physical Therapy, vol. 48, no. 9, 2018, pp. 676–684., doi:10.2519/jospt.2018.7426.
Baseball Specific Screening
The OnBase University screening stems from the belief that there is not only one technically correct way to play baseball or softball. There are an infinite number of ways to play the game. The best baseball players in history don’t all hit or pitch the same way, but they do have some commonalities in their styles that have allowed them to be the best. The aim of a good coach or trainer is to find the one efficient style that works for that player, and that is based on what the player can physically do. If we can match an athlete’s physical ability to his/her technical skills, it will help the player play at his/her highest level possible.Coach and Player Goals: To be Efficient and PowerfulWhat makes a hitting or pitching style Efficient?
It is ReproducibleThe player has command over their pitching/hitting styleThe player is able to maximize his/her power with the least amount of effort
What makes a hitting or pitching style Powerful?
Proper Kinematic Sequencing: how energy is transferred from the ground through the body to the ball or bat
It’s up to the coaches to guide the player into what kind of hitting or pitching style the athlete uses. Our goal is to assist the coach and player by determining how the athlete’s physical abilities relate to their technical skills. Pitching and hitting requires involvement from the whole body, from the feet all the way through to the neck, shoulders, elbow and hand. If there is a breakdown anywhere in this chain, it could lead to poor power, poor contact on the ball for hitters, inconsistency, and pain or injury. How is your body limiting your performance and where exactly are the breakdowns? That’s what we want to find out.How do we determine where the breakdowns are?Through Movement Screening: Functional Movement Screening (FMS), Y balance testing, OnBase University pitching and hitting screening, the Selective Functional Movement Assessment (SFMA), and through joint by joint assessment.We will provide these findings to you, your pitching or hitting coach, and your fitness coach to develop a team approach in order to help you become a better athlete.Let us help you and your coaches. Call us at 407-718-0437 or email us at rachel@jsportsrehab.com..Reference: http://www.onbaseu.com